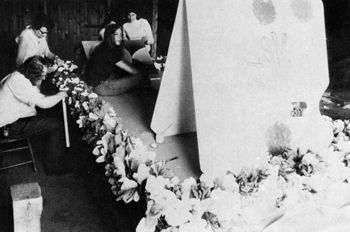
Patients Working on a Float for the Fourth of July circa 1970
|
Patients Working on a Float for the Fourth of July circa 1970 |
By
1970 the department of mental health was concerned mainly with creating
a social role for patients and providing effective services. Vermont hospitals
and institutions aimed to bring patients to a stable point where they could
then leave the hospital and “experience self-growth in a realistic
setting.” As the average daily population at the Vermont State Hospital
(VSH) fell and the number of both admissions and discharges increased, these
goals seemed to be realistic and clearly attainable; gone were the 1920s,
an era when insane persons were committed for life and kept separate or
hidden from the community. Now, fifty years in the future, treatment had
become much more rapid and effective, patient stays were shorter and shorter,
and the hospital found it increasingly easy to sew connections to the greater
community. |
Community Mental Health Services (CMHS) also played a major role in fostering ties between Vermont’s mental hospitals and its communities. Though the first of these centers were opened as early as 1957, they were, by 1970, finally playing a major role in the care and treatment of Vermont’s mentally afflicted. Divided among 5 regions throughout the state (to more easily organize administrative duties), the CMHS assisted patients in their transitions from hospital (especially VSH) back to normal life. As these clinics became more and more used, the rates of readmissions at both VSH and Brattleboro fell drastically. The 11 Community Mental Health Services that existed in 1968 offered services such as group therapy, out-patient care, partial hospital programs, and daycare. Each clinic consisted of 3 program levels: direct treatment, indirect consultation services, and preventative services.
|
| Brattleboro In 1970 the Brattleboro Retreat’s greatest problem was the financial crisis in which the institution found itself. In the years since 1960, the financial deficit had grown significantly, and this growth was attributed to a number of different factors. There was a 36% increase in staff numbers following the Medicare/Medicaid approval by federal funds in 1966, and since 1960, the number of employees had doubled. In the same period, the number of patients was halved, and the average length of stay fell to 4 to 6 weeks, compared to 4 to 6 months in 1960. The increased staff also enjoyed more benefits than ever before, including a work week capped at 40 hours, an increased minimum wage, pension plans, and insurance; each of these changes cost the hospital.
|
|
| Despite the Retreat’s struggles, however, positive aspects also arose from the changes. The increased staff and decreased number of patients, for example, created a close knit teamwork atmosphere between members of all departments throughout the institution. Additionally, Superintendent J. Douglas Sharpe and other hospital administrators were actively planning ways to put the hospital on the road to economic recovery. Ideas included the transfer of state patients (whom the Retreat had traditionally treated at less than audited cost) back to the State Hospital at Waterbury, and the simultaneous transfer of mentally retarded individuals from the Brandon Training School to Brattleboro. | |
The out-patient clinic was also proving very successful and profitable. In the 4 years leading up to June, 1960, the number of hours spent with out-patients increased from 1781 to 2087. The number of patients referred to the out-patient clinic from the in-patient hospital also increased, as did the revenue brought in by the out-patient clinic ($15,055.35 to $24,800.36). |
|
 Annual Summer Fun Festival circa 1970 |
Vermont State Hospital In striking contrast to the situation at Brattleboro, the State Hospital at Waterbury was experiencing a number of equally significant, but opposite changes. VSH saw a marked increase in business, characterized primarily by the high number of additions to the hospital, including admissions, readmissions, and returns. By the end of the biennial, these total additions surpassed the resident patient population. Demographically, the patient populations under the ages of 25 and 15 both doubled, and the patient population over age 65 decreased by 25%. Alcohol admissions were up, and the number of deaths was down. This increased workload placed increasingly steep demands on the staff. Vermont Mental Health Law Number 305, which went into effect in 1968, contributed significantly to these increased admissions. The law stated that there would be no financial bars to admissions and guaranteed the protection of civil rights to all patients, and as a result, voluntary admission increased by more than 50%. |
| To
cope with the increased workload, the hospital acquired more professional
personnel and staff, including trained psychologists, socials workers, and
nurses. The teaching hospital also expanded and there were many more students
and amateurs assisting doctors and nurses throughout the hospital. The new
psychiatric aide and psychiatric technician training programs were two other
major factors in the hospital’s success during this time of increased
pressure and workload. These programs provided the hospital with highly
trained nurses and technicians, and though there was no official licensure
received upon program completion, the administration appealed to the Vermont
Psychiatric Technicians Association to reverse this situation. |
| In
1970, each clinical team at the hospital had an established psychiatric
technician specialist to aid in the organization and development of ward
therapy programs. In addition to continuing individual and group psychotherapy,
family therapy and art therapy programs were developed. |
Patients Participating in Group Therapy circa 1970 |
| In addition to the actual people running the hospital, a computer terminal that could access computers throughout the hospital was developed, and this contributed greatly to the hospital’s organization and functioning. The ability to keep computerized progress notes proved highly useful in the face of such high patient admissions and populations. There were plans for the computer system to expand in the future into a medical record system and a system which could receive applications. The Community Mental Health Services also helped VSH adapt to the increased workload. The hospital and the local clinics worked together in a “cooperative effort” to provide the highest possible quality of care for in-patients, out-patients, and transitioning patients. In the 1970 biennial report there were three main recommendations for improvement throughout VSH. First, Support Services and Administration of the hospital needed to become more centralized and standardized to better and more efficiently handle the increasing workload at the hospital. Second, the Patient and Clinical Services needed to become more decentralized, also to better handle the rising volume of patients seeking care and treatment. This second objective could be at least partially met by making greater and greater use of the Community Mental Health Services throughout Vermont. Finally, some buildings, grounds, and equipment around the hospital were in need of maintenance. VSH patients, employees, and administration were prepared to work together to make the necessary repairs; the hospital legislature contributed to these efforts by designating $400,000 for maintenance work. In the coming years, the Vermont State Hospital aimed to recruit more personnel and to maintain and improve treatment programs that easily and effectively handled large numbers of patients. |
|